Introduction
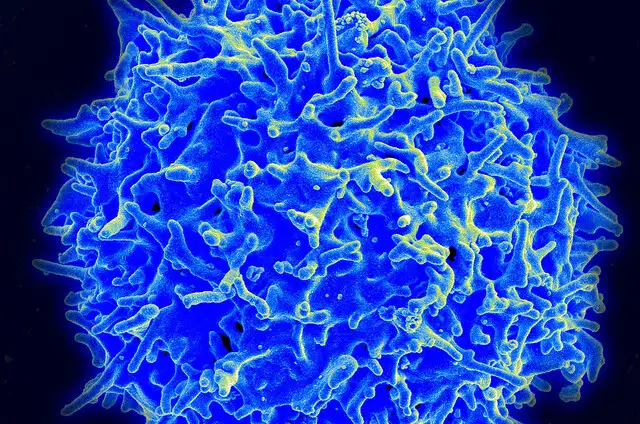
Immune checkpoint blockades (ICBs) have transformed the treatment landscape for advanced cancers. Despite their initial success, the effectiveness of ICBs has plateaued due to therapeutic resistance. This resistance hinders tumor-infiltrating lymphocytes (TILs), rendering them ineffective against cancer cells.
For clinicians, the challenge lies in reversing this resistance and reinvigorating TILs to effectively target tumor cells within the hypoxic tumor microenvironment caused by abnormal tumor vasculature.
Key Findings on HIF1α in Cancer TherapyIn a groundbreaking study published in Nature Communications, Dr. Lewis Zhichang Shi and his team at the University of Alabama at Birmingham unveiled the critical role of hypoxia-inducible factor 1-alpha (HIF1α) in T cell activation. HIF1α facilitates the induction of interferon-gamma (IFN-γ), a cytokine essential for triggering the tumor-killing capacity of T cells, even in oxygen-deprived conditions.
The Role of Glycolysis in T Cell ActivationUnder normoxic conditions, IFN-γ production in T cells is mediated by LDHa, a downstream target of HIF1α. However, in hypoxic environments, HIF1α becomes indispensable for initiating glycolysis and subsequent IFN-γ production. The UAB researchers used genetic mouse models, 13C-labeled glucose tracing assays, and pharmacological interventions to demonstrate that deleting HIF1α in T cells disrupts this metabolic shift and suppresses IFN-γ induction.Impact on Tumor Cell Killing and ICB TherapyThe absence of HIF1α in hypoxic T cells significantly reduced their ability to kill tumor cells in vitro and diminished the efficacy of ICB therapy in vivo.
The researchers observed that HIF1α-deleted T cells experienced metabolic disruptions, including depleted acetyl-CoA levels and impaired activation-induced cell death (AICD).A Breakthrough Solution: Acetate SupplementationThe study revealed that acetate supplementation could restore intracellular acetyl-CoA levels, reengage AICD, and rescue IFN-γ production in HIF1α-deficient T cells. This approach proved effective in overcoming ICB resistance.
Tumor-bearing mice with HIF1α-deficient T cells demonstrated significant tumor suppression and reduced tumor weights when treated with acetate supplementation and ICB therapy.ConclusionThe findings highlight the metabolic tug-of-war between TILs and tumor cells in the hypoxic tumor microenvironment. Strategies like acetate supplementation to bolster TIL metabolism and restore IFN-γ production offer a promising avenue to overcome ICB resistance. This research underscores the critical role of HIF1α in T cell function and its potential as a target for enhancing cancer immunotherapy.


















+ There are no comments
Add yours